Disruptive Mood Dysregulation Disorder(DMDD): Causes, Symptoms, Diagnosis, Treatment:
Overview:
Disruptive Mood Dysregulation Disorder (DMDD)
primarily affects children and adolescents and is characterized by severe and
recurrent temper outbursts disproportionate to the situation. These outbursts,
verbal or behavioral, are caused by irritability or anger between them.
Diagnosis requires frequent outbursts (at
least three times a week) in multiple settings. DMDD starts before age 10 and
can persist for years, impairing functioning, relationships, and academic performance.
DMDD often coexists with anxiety disorders, ADHD (hyperactivity disorder/Attention-deficit ), and ODD (Oppositional defiant disorder).
How common is DMDD?
Disruptive mood dysregulation disorder is a comparatively
new diagnosis, so research is required to determine just how common it is.
Early research shows that it may affect approximately 2% to 5% of children in
the U.S.
Who does DMDD affect?
Disruptive Mood Dysregulation Disorder (DMDD)
mainly affects children and adolescents. DMDD is a mental health disorder that
typically manifests during childhood, often before the age of 10. The symptoms
of DMDD, including frequent and intense temper outbursts and persistent
irritability, are predominantly observed in children within this age range.
What are the Symptoms of DMDD?
DMDD is characterized by symptoms that
primarily revolve around severe and repetitive temper outbursts that do not
align with the child's developmental stage. Here are some notable symptoms
commonly associated with DMDD.
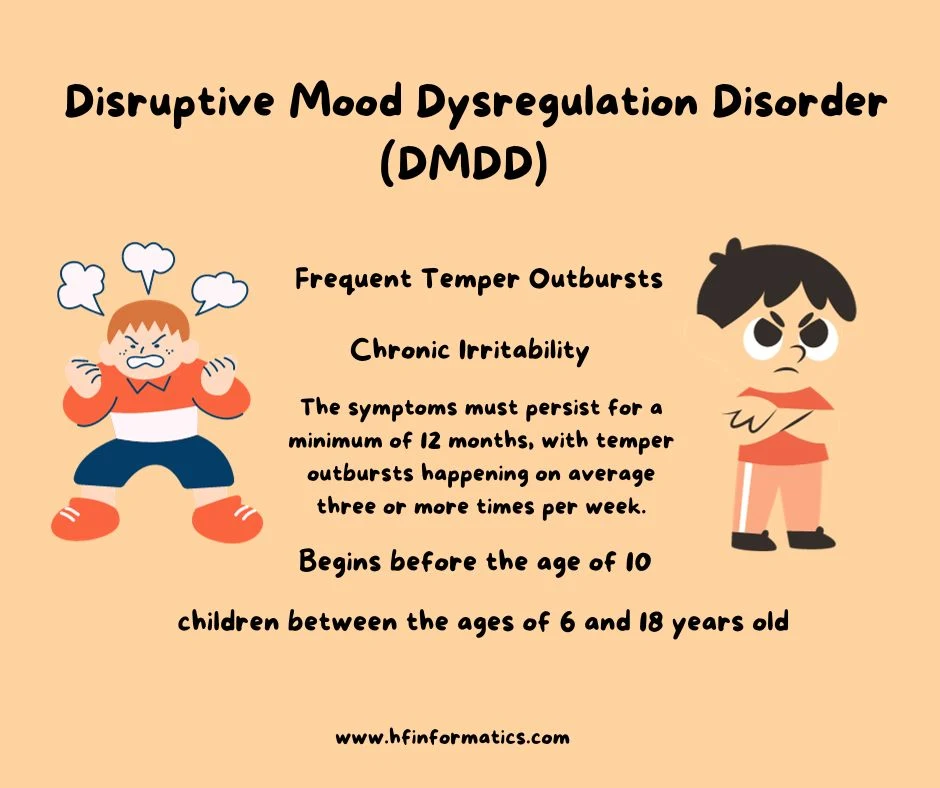
1. Frequent Temper Outbursts:
Children with DMDD experience frequent and
severe temper outbursts that are disproportionate to the situation. These
outbursts can be verbal (e.g., yelling, screaming) or behavioral (e.g.,
physical aggression, breaking objects).
2. Chronic Irritability:
Children with DMDD often show a persistent short-tempered
or angry mood most of the day, nearly every day. This irritability is present
between the temper outbursts and can be observed by others.
3. Duration and Frequency:
For a diagnosis of DMDD, the symptoms must
persist for a minimum of 12 months, with temper outbursts happening on average
three or more times per week. Additionally, these symptoms should be evident in
at least two different settings, such as the home and school environments.
4. Age of Onset:
DMDD typically begins before the age of 10,
and the symptoms may persist for several years.
What is the age range of Disruptive Mood Dysregulation Disorder?
The age range for Disruptive Mood Dysregulation Disorder (DMDD) typically begins in childhood and extends into adolescence. DMDD is typically diagnosed in children between the ages of 6 and 18 years old. The symptoms of DMDD usually emerge before the age of 10. It's important to note that DMDD is not typically diagnosed in adults, as the symptoms tend to diminish as individuals reach adulthood. However, if symptoms persist or new symptoms arise in adulthood, it is crucial to consult a mental health professional for a complete evaluation and appropriate diagnosis.
What is the difference between bipolar and DMDD?
Bipolar disorder and DMDD are two separate mental health conditions that share similarities in mood dysregulation, but they also have major differences. Let's explore some important contrasts between bipolar disorder and DMDD and keep reading:
1. Age of Onset:
Bipolar disorder usually emerges in
adolescence or adulthood, while DMDD is mostly diagnosed in children and
adolescents. DMDD symptoms typically initiate before the age of 10.
2. Mood Episodes:
Bipolar disorder is characterized by
different episodes of mania or hypomania (elevated mood) and depression. These
episodes can last for days, weeks, or even months. In contrast, DMDD is
characterized by chronic irritability, frequent temper outbursts, and
persistent anger, rather than distinct mood episodes.
3. Duration of symptoms:
Bipolar disorder involves longer
periods of mood disturbance, whereas DMDD symptoms are more persistent and
occur throughout the day.
4. The Severity of symptoms:
Bipolar disorder is often associated
with more severe mood swings, including extreme highs (mania) and lows
(depression). DMDD, on the other hand, is characterized by severe temper
outbursts that are disproportionate to the situation.
5. Treatment approaches:
Bipolar disorder is typically
managed with mood stabilizers, antipsychotics, and psychotherapy. DMDD
treatment may involve a combination of therapy, behavioral interventions, and
support for the child and their family.
It's important to consult a mental health professional
for an accurate diagnosis and appropriate treatment options. They will consider
the individual's symptoms, age, and other factors to determine whether bipolar
disorder or DMDD is the most appropriate diagnosis.
What causes disruptive mood dysregulation disorder?
As DMDD is a relatively new diagnosis,
researchers don’t have much insight into what causes it. Like oppositional
defiant disorder (ODD) and bipolar disorder (BD), DMDD likely develops from a
complex combination of biological, genetic, and environmental factors.
Diagnosis and Tests:
How is DMDD diagnosed?
Mental health professionals diagnose disruptive
mood dysregulation disorder if your child meets the condition’s criteria as
described in the Diagnostic and Statistical Manual of Mental Disorders(DSM-5) for at least 12 months. The DSM-5, published by the American Psychiatric Association,
is the standard reference book for recognized mental illnesses.
Your child will likely need to see a child
and adolescent psychologist or psychiatrist if
they’re showing signs of DMDD. These mental health professionals use specially
designed interview and assessment tools to evaluate your child for a mental
health condition.
Psychiatrists and psychologists often rely on
reports from the child’s parents, siblings, friends, and teachers to get a full
understanding of their behavior.
DMDD can occur at the same time as other
conditions associated with irritability, such as attention-deficit/hyperactivity disorder (ADHD) or anxiety disorders. Your child’s psychologist or psychiatrist will
carefully assess your child to develop an accurate diagnosis.
Management and Treatment:
What is the treatment for disruptive mood dysregulation disorder?
As DMDD is a newly recognized condition, there
haven’t been many research studies on its treatment. Current treatments are
mainly based on research focused on other childhood conditions associated with
irritability, such as anxiety and ADHD. The good news is that many of these
treatments also work for DMDD.
The two main treatment options for DMDD are
psychotherapy (talk therapy) and medications. In many cases, healthcare
providers recommend psychotherapy first before trying medications.
1. Psychotherapy:
Psychotherapy, also called talk therapy, is a term for a variety of
treatment techniques that aim to help a person identify and change unhealthy
emotions, thoughts and behaviors.
Psychotherapy takes place with a trained,
licensed mental health professional, such as a psychologist or psychiatrist. It
can provide support, education, and guidance to your child and/or your family
to help them with DMDD.
Different types of psychotherapy that may help
with DMDD include:
2. Cognitive behavioral therapy (CBT):
CBT is one of the most common forms of
psychotherapy. During CBT for DMDD, a mental health professional helps your
child take a close look at their thoughts and emotions. Your child will come to
understand how their thoughts affect their actions. Through CBT, your child can
unlearn negative thoughts and behaviors and learn to adopt healthier thinking
patterns and habits. The mental health professional can help your child
increase their ability to tolerate frustration without having an outburst.
3. Dialectical behavior therapy (DBT):
DBT is based on CBT, but it’s specially adapted
for people who experience emotions very intensely. DBT may help your child
learn to regulate their emotions and avoid extreme or prolonged outbursts.
4. Parent training:
Your child’s provider may recommend combining
therapy for your child with parent training. This therapy teaches parents or
caregivers more effective ways to respond to irritable behavior, such as
anticipating events that might lead their child to have an outburst and
attempting to prevent it. Training also focuses on the importance of being
consistent with your child and using positive reinforcement to decrease
unwanted behaviors and promote healthy behaviors.
5. Medication:
Currently, the U.S. Food and Drug Administration
(FDA) hasn’t approved any medications specifically for treating DMDD. However,
healthcare providers may prescribe certain medications to help manage DMDD
symptoms, including:
a. Stimulants:
Providers traditionally prescribe stimulants for the
treatment of ADHD. Research suggests that stimulant medications may also
decrease irritability in children with DMDD.
b. Antidepressants:
Providers sometimes prescribe antidepressants to treat
irritability and mood issues that children with DMDD may experience. One study
suggests that citalopram when
combined with methylphenidate (a stimulant), can decrease irritability in
children with DMDD.
c. Certain atypical antipsychotic (neuroleptic) medications:
Providers sometimes prescribe
these medications to treat children with irritability, severe outbursts, or
aggression. Providers typically only prescribe these medications for DMDD if
all other treatment approaches have been unsuccessful.
All medications have side effects. It’s important to monitor your child for any side effects and talk to their provider if side effects develop.
Prevention:
Can DMDD be Prevented?
Although it might not be possible to prevent DMDD, recognizing and acting on symptoms when they first appear can minimize distress to your child and family. It can also help prevent many of the problems associated with the condition.
What is the prognosis for disruptive mood dysregulation disorder?
Children with DMDD can experience significant
issues in school, at home, and in social relationships.
If left untreated, children with DMDD are at high risk of developing depression and/or anxiety disorders in adulthood. Because of this, it’s important to seek help for your child as soon as possible if they’re showing signs of DMDD.
How can I help my child with DMDD?
If your child has disruptive mood dysregulation
disorder, aside from getting them professional care, you can help them and
yourself in the following ways:
a. Learn as much as you can about DMDD:
Talk to your child’s healthcare provider or mental
health professional. Ask questions about treatment options and new research on
DMDD.
b. Communicate regularly with your child’s healthcare provider:
It’s important to work
closely with your child’s provider to make treatment decisions that are best
for them.
c. Work with your child’s teacher or school counselor:
Together, you can develop strategies and
accommodations that can help your child thrive in school.
d. Take a time-out or break when needed:
If you’re about to make the conflict with your child
worse instead of better, take a break and step away. This also sets a good
example for your child. Support your child if they decide to take a break to
prevent escalating a negative situation.
e. Take care of yourself:
Maintain interests and hobbies that you enjoy and
manage stress. Try to work with and gain support from the other adults who are
interacting with your child.
When should my child see their healthcare provider?
If your child has been diagnosed with disruptive
mood dysregulation disorder (DMDD), and their behavior becomes more severe or
further disrupts family or school life, talk to their provider.
What are
some common mental health conditions that often coexist with Disruptive Mood
Dysregulation Disorder (DMDD)?
Common
mental health conditions that often coexist with Disruptive Mood Dysregulation
Disorder (DMDD) include anxiety disorders, Attention-Deficit/Hyperactivity
Disorder (ADHD), and Oppositional Defiant Disorder (ODD). These conditions
frequently occur alongside DMDD, meaning individuals with DMDD may also
experience symptoms of anxiety, difficulties with attention and hyperactivity,
and oppositional behavior. It is important to note that the presence of these
comorbid conditions can complicate the diagnosis and treatment of DMDD.
Consulting a mental health professional is crucial to accurately identify and
address these coexisting conditions, ensuring appropriate treatment and support
for the individual.
What is disruptive mood dysregulation disorder dsm-5?
According to the Diagnostic and Statistical Manual of
Mental Disorders, Fifth Edition (DSM-5), Disruptive Mood Dysregulation Disorder
(DMDD) is a mental health condition characterized by severe and recurrent
temper outbursts that are inconsistent with the child's developmental level.
Here are the key diagnostic criteria for DMDD as outlined in the DSM-5:
1. Severe temper outbursts:
The child exhibits
frequent temper outbursts that are grossly out of proportion to the situation
and inconsistent with their developmental level. These outbursts can be verbal
and/or behavioral.
2. Chronic irritability:
The child displays a
persistently irritable or angry mood most of the day, nearly every day, between
the temper outbursts. This irritability is observable in others.
3. Duration and frequency:
The symptoms of
DMDD must be present for at least 12 months, with the temper outbursts
occurring on average three or more times per week. The symptoms should be
present in at least two settings (e.g., home, school).
4. Age of onset:
DMDD typically begins before
the age of 10, and the diagnosis should not be made for the first time after
age 18.
5. Exclusion criteria:
The symptoms of DMDD
should not be better explained by another mental health disorder, such as
bipolar disorder or oppositional defiant disorder (ODD). Additionally, the
symptoms should not be a result of substance use or a medical condition.
It's important to consult a mental health professional
for an accurate diagnosis and appropriate treatment options if you suspect DMDD
in yourself or someone else. They will conduct a comprehensive evaluation to
determine if the symptoms meet the criteria outlined in the DSM-5.
Conclusion:
Children and teens who are constantly irritable
can be very challenging for parents. While it’s normal for young children and
teens to show moodiness from time to time, frequent and disruptive behavior may
indicate disruptive mood dysregulation disorder (DMDD).
Starting treatment early for DMDD is important,
and the first step to treatment is to talk with a healthcare or a mental health
provider. Don’t be afraid to ask your child’s provider questions. They’re
available to help.
FAQs:
Q. What are the DSM-5 criteria for disruptive mood dysregulation disorder?
A. The criteria for DMDD are primarily based on those
developed for SMD, with some modifications. Criteria for DMDD includes, the severe, recurrent (≥3 times/week) temper outbursts (verbally
and/or behaviorally) that are grossly out of proportion in intensity or
duration to the situation, and inconsistent.
Q. What was the main reason for the DSM-5 addition of the diagnosis of disruptive mood dysregulation disorder for children?
A. Researchers at the National
Institute of Mental Health (NIMH) developed the DMDD diagnosis to diagnose
more accurately youth who may have been previously diagnosed with pediatric
bipolar disorder (despite not experiencing the symptoms needed for a
diagnosis of bipolar disorder).
Q. What does DMDD turn into as an adult?
A. If left untreated, children with DMDD are at high risk
of developing depression and/or anxiety disorders in adulthood.
Because of this, it's important to seek help for your child as soon as possible
if they're showing signs of DMDD.
Q. What is the V code for disruptive mood dysregulation disorder?
A. 81 Disruptive mood dysregulation disorder.




.jpg)
Post a Comment