Are Ear Infections Contagious? What You Need to Know:
Are Ear Infections Contagious?
Ear infections happen when fluid
accumulates in the middle ear and gets infected. They are most common in
children between 6 and 24 months old but can happen at any age. Ear pain due to
ear infection makes your infant or toddler irritable.
Most ear infections subside on their
own, but sometimes they require pain-relieving medications, antibiotics, or ear
tubes.
What is an Ear Infection?
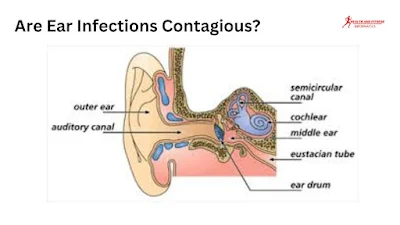
Ear infection also called
"otitis media," which means inflammation of the middle ear. The
middle ear is a small space behind the eardrum that is usually filled with air
and has tiny ear bones called ossicles. It's connected to the nose and throat
by a narrow canal called the eustachian tube. Otitis media happens when fluid
builds up in the middle ear and gets infected. The fluid builds up because the
eustachian tube doesn't drain properly.
How Ear Infection Occur?
An ear infection, also known as
“acute otitis media” is a sudden infection that occurs in the middle ear, an
air-filled space between your eardrum and inner ear. This part of the ear holds
delicate bones that pass on sound vibrations from your eardrum to your inner
ear, enabling you to hear.
Eustachian tubes are canals that
connect the middle ear to the back of your throat. They control air pressure in
the ear and impede fluid from accumulating in your middle ear space.
However, if the eustachian tube
doesn't function properly, fluid may have a hard time draining from your middle
ear space, causing muffled hearing. Ear infections caused by bacteria and
viruses can also lead to middle ear fluid. In such cases, the middle ear fluid
is infected and often causes discomfort in addition to muffled hearing.
Editor's Pick
How common are Ear Infections?
Acute otitis media is quite common,
especially in infants and toddlers. Childhood ear infections are the most
common illness other than colds. They affect children aged 6 months to 2 years
and are often common until your child is 8 years old.
Why are children more prone to get ear infections than adults?
There are several reasons why children
are more often affected by ear infections than adults such as:
- Children are more likely to catch infections from other kids.
- Their immune system (the body’s fighting system against infections)
- Their eustachian tubes don’t function as well as adults, and this encourages fluid to gather behind the eardrum.
Symptoms:
What are the symptoms of an ear infection?
Usually, ear infection symptoms
begin after a cold, including:
- Ear pain
- Trouble sleeping
- Loss of appetite
- Trouble hearing in the ear that’s blocked
- Brown, white, or yellow drainage from an ear. (This may indicate that your eardrum has broken.)
- A feeling of fullness or pressure in your ear
Don’t place anything in your ear
tube if you have drainage from your ear, as touching a torn or ruptured eardrum
can cause more damage.
How can I identify if my infant has an ear infection?
Since infants can’t communicate
their pain, it’s important to identify the signs. An infant or toddler with an
ear infection may:
- Tug or rub on their ears
- Cry more than usual or act irritable
- Mouth breathing
- Has a fever ranging from 100.5 to 104 degrees Fahrenheit (38 to 40 degrees Celsius). Half of children have fevers with ear infections.
- Have increased snoring or start mouth breathing
- Refuse to eat during feedings
- Your infant feels pressure in the middle ear changes as he swallows, causing more pain and less desire to eat.
Mouth breathing of your infant may
be a sign of enlarged adenoids. While, adenoids are small pads of tissue above
your throat, behind your nose, and near your eustachian tubes. Adenoids may
become infected/inflamed with the same viruses or bacteria that cause ear
infections.
Editor's Picks
Are Sinus Infection Contagious?
What causes an ear infection?
Viruses and bacteria cause ear
infections. Often, ear infections begin after a cold or another upper
respiratory infection. The germs travel
into your middle ear through the eustachian tube. Once inside, the bacteria or virus
can cause your eustachian tubes to swell. The obstruction of the eustachian
tube can lead to fluid build-up in the middle ear and poor tube function.
Are ear infections contagious?
Ear infections themselves are not
contagious, but the bacteria or viruses that can cause them can be. For
example, a cold or flu virus that spreads from person to person can lead to an
ear infection in someone already sick. Ear infection-causing bacteria can also
be transmitted through close contact with an infected person.
Repeatedly washing your child's hands
is crucial to prevent the spread of ear infection-causing bacteria and viruses.
Risks:
Risk factors for ear infections include:
Age:
Infants and toddlers are at a greater risk for ear infections.
Colds:
Having a cold elevates your
risk of developing an ear infection. Children in daycare and group settings are
at a greater risk of ear infections because they’re more likely to be around
children with colds or other contagious respiratory diseases.
Ethnicity:
Children of Native
American, Hispanic, and Alaska Native descent are more susceptible to ear
infections than children of other ethnicities.
Chronic illnesses:
Long-term
diseases such as immune deficiency, cystic fibrosis, and asthma, can increase
the risk of ear infections.
Smoky environments:
Exposure to
secondhand smoke elevates the risk of ear infections.
Complications:
What are the complications of ear infections?
Most ear infections don’t cause
long-term issues. When complications happen, they’re usually related to
repeated or ongoing ear infections. Complications include:
Children's language and speech
development can be significantly delayed by muffled hearing or hearing loss.
Hearing loss:
Short-term hearing loss or changes in your hearing (sound distortions or muffling) are common during an ear infection. Significant hearing loss can occur due to repeated or ongoing infections or damage to internal structures in your ear.
Torn eardrum:
About 5% to 10% of
kids with ear infections may experience a small tear in their eardrum.
Typically, the tear will heal on its own, but surgery may be required if it
does not.
Spread of the infection:
Untreated
infections or infections that don’t improve on their own can spread. Infection
can spread to mastoiditis (the bone behind your ear).
Diagnosis:
How is an ear infection diagnosed?
Healthcare providers can diagnose
ear infections in children by examining their symptoms and checking for signs
of a cold. Using an otoscope, they can look at the child's eardrum for inflammation,
swelling, or redness - all signs of an ear infection. Doctors may also use a
pneumatic otoscope to check for fluid in the middle ear. the eardrum will not
move easily. the eardrum will not move easily.
Editor's Picks
Huffing Side Effects Using Inhalants
Are there further tests my child may need?
Your child may need additional
tests, such as;
1. Tympanometry:
This test uses air
pressure to check for fluid in your child’s middle ear.
2. Tympanocentesis:
This procedure
allows your child’s provider to remove fluid from your child’s middle ear and
test it for viruses and bacteria. Their provider may recommend tympanocentesis
if other treatments haven’t cleared the infection.
3. Reflectometry:
This is to
use sound waves to check for fluid in your child’s middle ear.
4. Hearing tests:
This is a hearing test to determine if your child has hearing loss. Kids who have repeatedly or long-term ear infections or fluid in their ears that doesn't drain are more likely to have hearing loss
Treatment:
How is an ear infection treated?
Treatment depends on many factors,
such as:
- The severity of the infection
- Your child’s age
- The nature of the infection (first-time, constant, or repeat infection)
- Whether fluid stays in the middle ear for a long time
- Most, ear infections are cured without treatment.
Your child's condition may be
monitored by your healthcare provider to determine if improvement is occurring
before treatment is prescribed. Your child may need antibiotics or maybe
surgery for infections that don’t go away. Meanwhile, pain medicines can help
with symptoms like ear pain.
a) Antibiotics:
Your child might require antibiotics
if the ear infection is caused by bacteria. Healthcare providers might wait for
up to three days before prescribing antibiotics to observe if a mild infection
clears on its own. In cases of severe infection, your child may need to start
antibiotics right away.
Your healthcare provider may suggest
your child use over-the-counter (OTC) medicines like Motrin®, Tylenol®, or
Advil® to help with pain and lower fever. Sometimes, your doctor might
recommend ear drops to alleviate pain. It is essential to adhere to your
doctor's advice on which medications are safe for your baby. You should never give aspirin to your child
as it can cause a severe condition known as Reye's syndrome.
b) Ear tubes (tympanostomy tubes):
If your child keeps getting ear
infections, if the infections don't get better with antibiotics, or if they
have hearing loss due to fluid buildup, they might need ear tubes. A specialist
called ENT (an ear, nose, and throat) doctor puts in the tubes during a short
procedure called a tympanostomy, which takes about 10 minutes. Your child can
go home the same day.
Procedure:
During the procedure, the doctor
puts a small metal or plastic tube into a tiny cut in your child's eardrum.
This process, called a myringotomy, helps to make a hole in the eardrum and
drain the fluid. Once the tubes are in place, they help air get into the middle
ear and let the fluid drain. The tubes usually stay in place for 12 to 18
months. They might fall out on their own, or your child might need another
surgery to remove them. After the tubes are gone, the hole in your child's
eardrum will heal and close.
American Academy of Pediatrics Treatment Guide for Acute Otitis Media:
It is important to finish the entire
course of antibiotics even if symptoms improve. Stopping early may cause the
infection to return.
Prevention:
How can I prevent my child from ear infections?
Here are some ways to reduce your
child’s risk of ear infections:
- Breastfeed your baby, especially during the first six to 12 months. Antibodies in breast milk (chest milk) fight viruses and bacteria that cause infections.
- Avoid secondhand smoke. Avoid exposure to secondhand smoke, and don’t allow others to smoke around your child.
- Prevent colds and other respiratory illnesses. Be proactive in preventing colds, especially during your child’s first year. Teach them about regular hand washing and sneezing or coughing into their elbow. Don’t allow them to share food and utensils. If it’s an option, avoid large daycare centers until they’re older.
- Bottle-feed your baby in an upright position. If you bottle-feed, hold your child upright so their head is higher than their stomach. This position can prevent formula milk or other fluids from flowing backward and collecting in their eustachian tubes.
- Make sure your child gets all their vaccines on time, including the annual flu vaccine for kids 6 months and older. Talk to your child's doctor about vaccines for diseases like pneumococcal disease and meningitis.
Can an ear infection go away on its own?
Yes, many infections get better by
themselves. That's why your doctor might wait before giving you medicine like
antibiotics. In the meantime, you can use painkillers to help with things like
ear pain. Depending on how old your baby is, their symptoms, and their
temperature, they might need antibiotics to get better. If your child keeps
getting sick a lot, or if there's still fluid in their ear that could affect
their hearing, they might need ear tubes.
When should I consider a visit to my healthcare provider for an ear infection?
Visit your healthcare provider
immediately if:
- Your child’s walk isn’t steady.
- your child’s ear pain is severe
- Your child develops a stiff neck.
- Your child acts sluggish, looks or acts very sick, or doesn’t stop crying despite all efforts.
- your child has a fever above 104 degrees F
- You see bloody or pus-filled fluid draining from the ear.
- Your child shows symptoms of weakness in their face.
- Call your healthcare provider if:
- Ear pain isn’t better after three days of taking an antibiotic.
- A fever remains or comes back more than 48 hours after starting an antibiotic.
Conclusion:
Get in touch with your child's doctor if they have signs of an ear infection and they don't start feeling better in two to three days. Usually, ear infections improve without needing any treatment. But depending on how old your child is and what symptoms they have, they might need antibiotics. The doctor can also suggest pain relievers to help your child feel better while their body fights off the illness.




.jpg)
Post a Comment