Bicornuate uterus : How does it affect your pregnancy
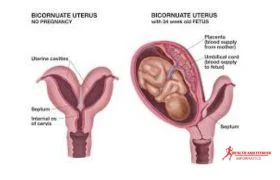
The bicornuate uterus is a congenital abnormality of the uterus. This heart-shaped, irregular form of the uterus is an uncommon condition. Most women with a bicornuate uterus can have a healthy pregnancy but may have slight risks of miscarriage.
Overview:
A bicornuate uterus means that the uterus is
either completely or partially duplicated, but there's only one cervix. The
health experts don’t know how this condition affects a woman's ability to have
children1.
Having a bicornuate uterus can lead to
miscarriage, preterm labor, and premature birth. Ultrasound can confirm the
diagnosis, but it’s crucial to note that having a bicornuate uterus doesn’t essentially
mean you can’t get pregnant, but it can be more challenging.
Healthcare providers treat a pregnancy in one
part of a bicornuate uterus using Stressman and cerclage metroplasty,
4.
What is a bicornuate uterus?
The health experts
define a bicornuate uterus as
“The bicornuate uterus
is a type of congenital uterine irregularity that happens due to a lateral
fusion defect of the Mullerian ducts during embryologic development.
This condition leads
to numerous anatomic variations such as complete or partial division between
the endometrial cavities, single or duplicated cervices, and associated vaginal
anomalies.
A woman with a
bicornuate uterus may be identified at the time of pregnancy, during the
evaluation of poor obstetrical outcomes, or evaluation of an obstructing, or
evaluation of an obstructing, or nono obstructing vaginal anomaly, still
several females are asymptomatic and remain undiagnosed. Evaluating females
with a possible uterine anomaly needs a physical examination and detailed
history4.
How common are uterine abnormalities?
Uterine abnormalities are quite common,
impacting approximately, 3-4% of females. But it’s not often that pregnancies
occur in a uterus with bicornuate uterus problems.
The occurrence of uterine differences varies, depending on the population and the diagnostic method. The occurrence of 1-10% was found in an unselected population 2-8% in subfertile females, and 5-30% of females with a history of miscarriage.
How can I know if I have a bicornuate uterus?
You don’t even know you have a bicornuate
uterus until your healthcare provider tells you after a check-up for the
problem of something else, such as, during a routine pregnancy check-up or even
during childbirth, your healthcare provider may discover that your uterus is
shaped differently3.
What should my healthcare provider consider if I have bicornuate uterus?
Your healthcare provider should consider
certain possibilities, such as having painful periods or having multiple
miscarriages. It’s also crucial for you if you are trying to conceive and are
having trouble.
A study found that about 3% of women with
uterine problems have a bicornuate uterus, where the uterus is heart-shaped.
Another study came across children born to
mothers with this condition and revealed that they were more likely to have
birth defects.
Is it possible to become pregnant if I have a bicornuate uterus?
Your pregnancy can be difficult if you have
bicornuate uterus. Although it’s possible to get pregnant there will be a higher
risk of complications such as miscarriage, or preterm labor. Your ultrasound
report will confirm the diagnosis, but it’s important to know that having this
condition doesn’t necessarily mean women can’t get pregnant—it just might be more challenging.
Editor's pick
What is circumvallate placenta? symptoms, causes, diagnosis, treatment
Subclinical hypothyroidism in pregnancy
Why does a bicornuate uterus cause difficulty in getting pregnant?
The problem is not
usually getting pregnant—it’s carrying the
baby to full term. Women with uterine issues might have smaller uteruses,
weaker muscles, or problems with blood flow, all of which can make it harder
for the baby to grow properly. This can lead to miscarriage, the need for a
C-section, or premature birth.
Symptoms:
What are the symptoms of bicornuate uterus?
You might experience
certain symptoms if you have a bicornuate uterus such as:
- Vaginal bleeding
- Pelvic pain
- Frequent miscarriages
- Painful intercourse (dyspareunia)
- Painful menstruation
In most cases, you may
even don’t know you have a heart-shaped uterus and you may feel normal with
these symptoms. Your ultrasound report can reveal your uterus anomaly.
Causes:
What causes a bicornuate uterus?
A bicornuate uterus is a congenital condition,
meaning that it develops in the womb between 10 and 20 weeks of pregnancy. A heart-shaped uterus characterizes this uterus
anomaly
During fetal development, the Mullerian ducts, which are two ducts that typically merge to form one uterine cavity, may not fuse completely in some individuals. This results in forming a bicornuate uterus, which has two uterine cavities. This condition can manifest as a deep heart shape or a minor malformation that never causes any issues. It is important to note that a heart-shaped uterus is not hereditary, which means that it cannot be passed down from parent to child.
Diagnosis:
How is a bicornuate uterus diagnosed?
Most females don’t
know that they have a heart-shaped uterus until they experience repetitive
miscarriages. Your healthcare provider can reveal the shape of your uterus
after repeated pregnancy loss, during pregnancy, or because of painful periods by
following tests such as:
1. Ultrasound:
Overall, ultrasound is a non-invasive and
valuable tool in the diagnosis of bicornuate uterus, providing crucial
information for healthcare providers to effectively manage and counsel patients
with this condition.
In the case of bicornuate uterus, ultrasound
can accurately identify the characteristic heart-shaped or
"bicornuate" appearance of the uterus. This imaging technique can
differentiate between a bicornuate uterus and other uterine abnormalities, such
as a septate uterus or a unicornuate uterus.
2. MRI (magnetic resonance imaging):
MRI is another imaging modality that can be used in the
diagnosis of bicornuate uterus. While ultrasound is typically the first-line
imaging technique for evaluating uterine abnormalities, MRI can offer
additional information and detail, especially in complex cases or when
ultrasound results are inconclusive.
MRI provides highly detailed images of the internal structures
of the body, including the uterus. It can accurately delineate the shape, size,
and configuration of the uterus, allowing for a comprehensive assessment of
uterine anomalies such as bicornuate uterus.
Why is appropriate imaging important when diagnosing a bicornuate uterus?
Doctors use special tests like imaging to tell
if a woman has a bicornuate uterus or another kind of problem with her womb.
They also might check her urinary tract with these tests. Even though having a
bicornuate uterus usually doesn't make it harder to get pregnant, it can make
some problems more likely during pregnancy4.
Treatment:
What are the treatment options for bicornuate uterus?
The management of a bicornuate uterus
varies depending on factors such as the severity of the condition, symptoms,
and the patient's reproductive intentions. Treatment options typically include:
1. Symptomatic Treatment:
Women experiencing symptoms
such as heavy menstrual bleeding or pelvic pain may benefit from symptomatic
treatment options, including medications or surgical procedures to alleviate
discomfort.
2. Pregnancy Management:
Close monitoring and management
of any pregnancy-related complications are crucial for women with a bicornuate
uterus. This involves regular prenatal care and interventions such as cerclage
to prevent preterm labor.
3. Fertility Assistance:
For women experiencing difficulty
conceiving, assisted reproductive technologies like intrauterine insemination
(IUI) or in vitro fertilization (IVF) may be utilized to improve the chances of
pregnancy.
4. Surgical Correction:
In cases where the bicornuate
uterus significantly impacts fertility or increases the risk of complications
during pregnancy, surgical intervention may be considered. Metroplasty, a
procedure to remove the uterine septum, can often improve fertility outcomes
and reduce the risk of miscarriage or preterm birth.
5. Observation:
If the bicornuate uterus is asymptomatic
and does not interfere with fertility or pregnancy, a watch-and-wait approach
may be recommended. Regular monitoring by your healthcare provider ensures any
potential complications are detected early.
When might healthcare providers recommend surgical intervention?
For some women
who've had a lot of pregnancy problems before, doctors might think about doing
surgery to help them. They might do a surgery called Strassman metroplasty or
put in something called a cervical cerclage4.
What complications may arise from surgical treatment for a bicornuate uterus?
When treating a
bicornuate uterus through surgery, there will be some associated risks,
including:
- Infection
- Bleeding
- Uterine scarring/adhesions
Prevention:
How can I prevent a bicornuate uterus?
A bicornuate uterus is a condition that arises during
fetal development and is not caused by anything your parents did or didn’t do.
Therefore, there is nothing you can do to prevent a heart-shaped uterus.
How will a bicornuate uterus affect my pregnancy?
The heart shape of your uterus does lead you to some
extended higher risk for certain pregnancy complications including;
- Low birth weight (because your fetus doesn’t have enough space to grow)
- Preterm birth and early labor
- Miscarriage
- Postpartum hemorrhage
- Vaginal bleeding
- The fetus is transverse, breech, or in another position in the uterus other than head-down.
- Incompetent cervix
- Placenta previa, or other condition of the placenta
- Elevated chance for cesarean delivery
- Pregnancy-induced high blood pressure
Pregnancy with a bicornuate uterus requires more
monitoring compared to a pregnancy with a normal uterus shape. Your healthcare
provider will likely have a more prenatal ultrasound so they can observe the
shape and size of your uterus and the position of the fetus, placenta, and
shape.
The chances of having a c-section can elevate with the
heart-shaped uterus as your baby is more on the verge of the breech.
Can I have a normal childbirth with a bicornuate uterus?
You can have a healthy pregnancy and normal childbirth.
You need to practice extra precautionary measures and regular check-ups to
ensure you and your baby stay safe through pregnancy and delivery.
Can a bicornuate uterus affect my labor and delivery?
Your heart-shaped uterus could affect your childbirth.
Since your uterus is abnormal in shape, it might not enlarge enough to accommodate
a full-term baby. This means your baby could be jam-packed very tightly and in
an uncomfortable position inside your womb. As a result, there will be higher
risks of your baby being breech. Therefore, healthcare providers often
recommend a C-section.
Will my baby have a birth defect?
It's important to note that having a bicornuate uterus
does not necessarily mean that your baby will have a birth defect. However, it
does increase the likelihood of preterm labor, which means that you may give
birth before your baby's organs or systems have fully developed, typically
before the 37th week of pregnancy.
Conclusion:
The bicornuate
uterus is a heart-shaped anomaly of the uterus and presents as a rare
congenital uterine anomaly. Although most women with this condition can have
healthy pregnancies, there is a slight risk of miscarriage. While imaging aids
in diagnosis, there's limited knowledge about its impact on fertility.
Pregnancy complications, such as preterm labor, are heightened, warranting
careful management, including surgical interventions for select cases.





.jpg)
Post a Comment